Is proton beam therapy the future for cancer treatment?
(If physicists are so smart, why don’t you cure cancer? “We do” – Fermilab particle physicist GP Yeh)
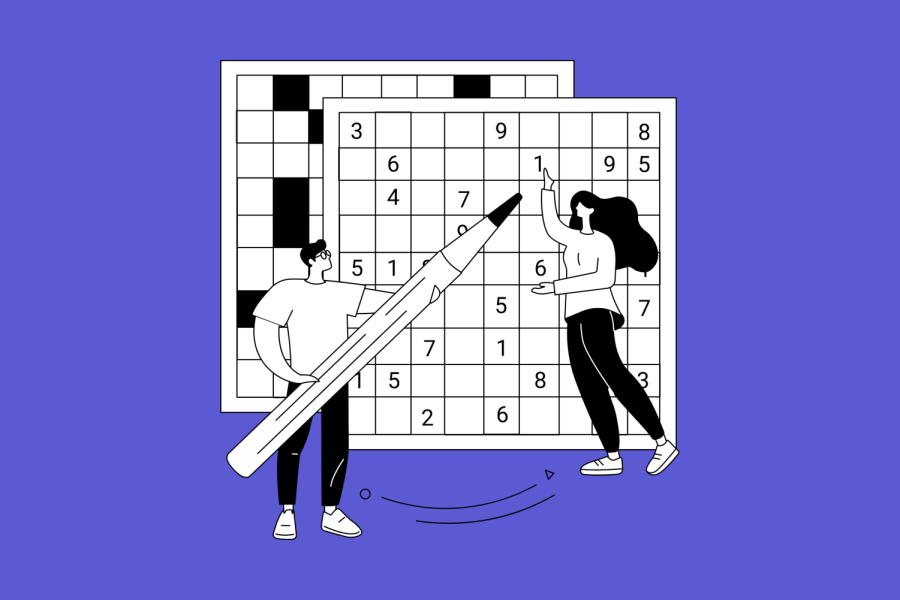
Dr. William Hartsell medical director of Northwestern Medicine Chicago Proton Center in Warrenville planning treatment to use protons to break down a patient’s tumor (photo provided by Northwestern Medicine)
November 21, 2019
Tiny, colorful handprints decorate a patient room wall at Northwestern Medicine Chicago Proton Center in Warrenville. Each one signed by a child whose life was saved through proton beam cancer therapy.
“When I follow-up with brain tumor patients, I know what I used to see,” said radiation oncologist Dr. William Hartsell, who explained how damaging traditional radiation therapy can be for children. “But the kids we treated (with proton therapy) are doing so much better. Their quality of life is better.”
Hartsell serves as the center’s medical director, specializing in particle cancer treatment. He said while standard radiation therapy helps break down tumors, its indiscriminate energy also causes damages to the patient’s healthy cells. Because children have rapidly developing tissues, this radiation damage can prevent their cells from repairing, causing future developmental problems and a higher risk of secondary tumors.

“One of the huge advantages of proton therapy is we give less of a dose to the healthy tissues around the area we are treating,” said Hartsell. “Protons give off most of their energy (in a quick burst) precisely where we direct them on the tumor, and nothing beyond it. This is important for developing children, but also for adults whose tumor is near critical structures in the body and requires precision to prevent harm. Adult tissues normally repair, but problems resulting from radiation can cause future secondary cancerous mutations.”
While not preferred for all cancers, like breast cancer or leukemia, where traditional therapies are more viable, proton therapy is recommended for tumors in sensitive areas like the brain stem, spinal cord, heart, lymph glands, eyes, kidneys, liver and lung tissues. Mutations caused by radiation can increase the chance of heart attack, and scarring can impair organ function. Proton therapy’s protection of healthy tissue dramatically reduces the risk for these side-effects.
Hartsell’s practice currently treats around 5,000 patients a year, with 10% of those receiving proton therapy. He said ideally, insurance would allow them to treat the 15% of patients with tumors requiring the most precision. Since treatment began in 1990, 65,000 patients have been treated in America and over 130,000 worldwide.
After completing his final proton treatment for prostate cancer, Dick Hill, 77, a retired consultant and human resources expert, believes this modern treatment is the only way for patients to go.

“After I was diagnosed, I researched all my options and discovered that proton therapy, like modern electric cars versus old gas automobiles, is vastly superior,” said Hill. “Patients have the bias of traditional radiotherapy’s industry working against them. You need to take charge of your own diagnosis and find someone who is on top of current research. With proton therapy, I was able to use a new form of tumor scanning, leading to even more precision with no side-effects, besides exhaustion.”
CNN reports many doctors argue standard treatments are just as effective as proton therapy at much less the cost.
Hill received treatments at the Proton Center the standard five days a week, for a total of 33 treatments for his specific cancer. His body is currently free of cancer. He believes because standard therapy is so invested with millions of dollars in equipment and thousands of people trained, the medical world and insurance companies are slow to embrace proton therapy. With the treatment’s high price, he considers himself lucky to have been approved by insurance through his wife’s state plan as a retired teacher.
“I was nervous (entering treatment), but gained great confidence in how thorough the imaging and planning was in setting me up for my treatments,” said Hill. “Medical students should pursue proton therapy so they can be on the cutting-edge of scientific theory and research. There are constantly new developments; this is where there’s going to be a tremendous future with growth potential.”
According to CNN, proton therapy is 60 percent more expensive than standard radiation therapy. Insurers get billed $25,000-$50,000 per course of treatment. This has led to around two-thirds of applications for proton therapy initially being denied by insurers who call the treatment “experimental.” A combination of the treatment’s high price, insurers’ denial rates, and the high cost of building facilities has prevented proton therapy from expanding more rapidly. There are currently only 32 proton beam centers in the U.S., but the number is steadily growing, with four more under construction.

Hartsell believes with over 130,000 patients treated worldwide and over 75 global centers, proton therapy shouldn’t be labeled “experimental.”
“Our treatment has been proven safe, is commonly done and is FDA approved,” said Hartsell. “(Insurers) can’t hide behind their definitions of ‘experimental’ and ‘investigational.’ The University of Texas found insurance policies in Texas have become more restrictive over time, and the insurers used fewer references in their medical policy. Current studies undermine what they are doing with their policies.”
Hartsell said imaging techniques are constantly getting even more proficient, allowing detection of the precise shape and small amounts of tumor cells. This allows physicians to simulate treatment on 3-D models. Once treatment begins, the beam of protons is generated by the cyclotron, which is a scaled-down version of the particle accelerator located at Fermilab National Laboratory in Batavia. The protons are steered down the beam line with magnets directing their flow into each of the four patient rooms. Doctors can direct the proton beam with carved shapes in brass matching the tumor, with waxy molds slowing down protons in certain areas to control depth of treatment. Doctors also use the more precise scanning technique called pencil beam.
“It’s almost like paint-by-numbers,” said Hartsell. “We direct the narrow beam at the specific part of the tumor we want to treat. The higher energy protons penetrate further than the lower-energy protons. We start deep and gradually lower the energy, covering the tumor layer by layer.”
“We (hope) to develop flash therapy where almost all the treatment is given instantaneously. This seems to have a lesser effect on normal tissues, yet the same intended effect on tumor tissues.”
Dr. Mark Pankuch, the Proton Center’s director of medical physics and dosimetry, said the treatment success depends on the coordination between the center’s physicians and medical physicists.
“My interest is in applied physics, and making these magnets for the protons and using them to apply cancer treatment to help patients is very exciting,” said Pankuch. “Every patient has a unique problem for us to overcome, so it never gets dull working here.”
Pankuch said the cyclotron’s constant magnetic field causes the protons to rotate and spin in a circular orbit. Once the protons reach their maximum velocity, they shoot out down the beam line. Focusing magnets direct the flow of protons into the patient’s room, and place the beam in the best position to access the tumor. The level of energy is manipulated for the need of treating each patient’s tumor.
Pankuch said constantly developing technology keeps the field exciting. Fermilab helps develop new technology, and Argonne National Laboratory in Lemont is currently developing a linear accelerator using heavy-ions for cancer treatment. He said costs can be decreased by using a superconducting system, which is twice as small as the cyclotron accelerator. These accelerators cost far less to operate.
Hartsell believes costs can be further decreased by building one or two-room centers, as opposed to their larger four-room center. This lower price will encourage more centers to be built. He said they are also focusing on maximizing precision to give more of the treatment and reduce the patient’s sessions. The standard used to be 44 treatments for prostate cancer. Hartsell said they can get it down to 28, and eventually they want 5 treatment sessions with the same outcomes.

GP Yeh, born in Taiwan, worked as a particle physicist at Fermilab for over 25 years, and was one of the leading advocates in building the proton center in Warrenville. Following studies by famous particle physicist Robert Wilson (1946), who noticed protons’ localized energy spikes after their velocity is slowed (described by the Bethe-Bloch Formula), the lab researched heavier neutron therapy for 30 years, starting in 1975. Using their scaled-down accelerator, the lab treated a few thousand people. In 1986, Loma Linda Hospital in California requested Fermilab to build the first scaled-down accelerator to be placed in a hospital. Hartsell said the success of this facility helped inspire the construction of the center in Warrenville.
“Physics is the basis of all sciences,” said Yeh. “The more physics you comprehend, the better you can understand everything in the universe. You have to lead the way and demonstrate by example. If you can show people a better way through science, industry will follow. National labs like Fermilab show the world the possibilities.”
“It shakes people when you threaten their business with new ideas. However, we can prove to hospitals that proton therapy can make them more money while also treating more patients.”
Yeh also helped advocate Taiwan to build three proton centers and one heavy-ion center. Yeh believes heavy-ion and boron nuclear capture therapy could also replace standard radiation treatment. Heavy-ion is used in Japan, and uses the nucleus of carbon, rather than protons, to deliver a charge 36 times stronger. This higher intensity reduces the amount of needed sessions, but also requires a bigger accelerator. There are currently only12 facilities in the world because construction costs around $250 million.
Cheaper than heavy-ion, boron treatment attaches boron to the tumor, which attracts neutrons to break up the tumor. Therefore, only tumor cells would be targeted by the low-energy neutron beam, leaving healthy cells undamaged. Tumors can often be treated in one session. The technology has currently treated over 1,000 patients. Yeh says its $10 million construction cost should incentivize hospitals to invest more in the technology.
Standard 4-room proton therapy centers cost around $15o million, however single room centers can be made for around $40 million.
Hartsell said improving cancer treatments should be seen as part of the physician’s Hippocratic Oath to do no harm to the patient. Because the second most common pediatric cancer is brain tumors, the safer method of proton therapy must be continually developed and expanded to ensure as many lives as possible can be saved.
(*Northwestern Medicine Chicago Proton Center offers training programs to radiologic technology students from the College of DuPage)
















Dick Hill • Nov 26, 2019 at 11:54 pm
JOEY: Congratulations on a GREAT article. You really mastered the Proton Radiation concepts & applications! I can tell from what Dr. Hetzell filled in for you (he is my Dr.) that you really “fired him up” — as he is normally not as passionate when he talks about proton therapy.
He is really a leader in the field & I think — “quite a guy.”
If you have an interest, I will send you his bio I found on the internet & my article that I wrote about my Proton Center experience. You truly are a gifted writer — very clear on a complex topic, your ideas flow together nicely & build into a complete, clear picture.
Good luck in whatever career you choose!
Dick H.
Robert Emery • Nov 23, 2019 at 10:20 am
University of Washington Medical Center in Seattle installed a particle accelerator in their hospital in 1984 and continues to treat with fast neutrons. It is the only facility in the US providing this treatment modality, which is more damaging to cancer tissue and more effective for certain types of cancer than photons or protons.